20/200 2.2 serial key or number

20/200 2.2 serial key or number
Social Security
The body system listings in parts A and B of the Listing of Impairments will no longer be effective on the following dates unless extended by the Commissioner or revised and promulgated again.
1. Low Birth Weight and Failure to Thrive (): June 12,
2. Musculoskeletal System ( and ): January 27,
3. Special Senses and Speech ( and ): April 24,
4. Respiratory Disorders ( and ): October 7,
5. Cardiovascular System ( and ): January 27,
6. Digestive System ( and ): January 27,
7. Genitourinary Disorders ( and ): December 9,
8. Hematological Disorders ( and ): May 18,
9. Skin Disorders ( and ): January 27,
Endocrine Disorders ( and ): June 26,
Congenital Disorders That Affect Multiple Body Systems ( and ): April 3,
Neurological Disorders ( and ): September 29,
Mental Disorders ( and ): January 17,
Cancer (Malignant Neoplastic Diseases) ( and ): July 20,
Immune System Disorders ( and ): January 17,
Part A
Criteria applicable to individuals age 18 and over and to children under age 18 where criteria are appropriate.
Sec.
Musculoskeletal System.
Special Senses and Speech.
Respiratory Disorders.
Cardiovascular System.
Digestive System.
Genitourinary Disorders.
Hematological Disorders.
Skin Disorders.
Endocrine Disorders.
Congenital Disorders That Affect Multiple Body Systems
Neurological Disorders.
Mental Disorders.
Cancer (Malignant Neoplastic Diseases).
Immune System Disorders.
Musculoskeletal System
A. Disorders of the musculoskeletal system may result from hereditary, congenital, or acquired pathologic processes. Impairments may result from infectious, inflammatory, or degenerative processes, traumatic or developmental events, or neoplastic, vascular, or toxic/metabolic diseases.
B. Loss of function.
1. General. Under this section, loss of function may be due to bone or joint deformity or destruction from any cause; miscellaneous disorders of the spine with or without radiculopathy or other neurological deficits; amputation; or fractures or soft tissue injuries, including burns, requiring prolonged periods of immobility or convalescence. The provisions of and notwithstanding, inflammatory arthritis is evaluated under (see D6). Impairments with neurological causes are to be evaluated under ff.
2. How We Define Loss of Function in These Listings
a. General. Regardless of the cause(s) of a musculoskeletal impairment, functional loss for purposes of these listings is defined as the inability to ambulate effectively on a sustained basis for any reason, including pain associated with the underlying musculoskeletal impairment, or the inability to perform fine and gross movements effectively on a sustained basis for any reason, including pain associated with the underlying musculoskeletal impairment. The inability to ambulate effectively or the inability to perform fine and gross movements effectively must have lasted, or be expected to last, for at least 12 months. For the purposes of these criteria, consideration of the ability to perform these activities must be from a physical standpoint alone. When there is an inability to perform these activities due to a mental impairment, the criteria in ff are to be used. We will determine whether an individual can ambulate effectively or can perform fine and gross movements effectively based on the medical and other evidence in the case record, generally without developing additional evidence about the individual's ability to perform the specific activities listed as examples in B2b(2) and B2c.
b. What We Mean by Inability To Ambulate Effectively
(1) Definition. Inability to ambulate effectively means an extreme limitation of the ability to walk; i.e., an impairment(s) that interferes very seriously with the individual's ability to independently initiate, sustain, or complete activities. Ineffective ambulation is defined generally as having insufficient lower extremity functioning (see J) to permit independent ambulation without the use of a hand-held assistive device(s) that limits the functioning of both upper extremities. (Listing C is an exception to this general definition because the individual has the use of only one upper extremity due to amputation of a hand.)
(2) To ambulate effectively, individuals must be capable of sustaining a reasonable walking pace over a sufficient distance to be able to carry out activities of daily living. They must have the ability to travel without companion assistance to and from a place of employment or school. Therefore, examples of ineffective ambulation include, but are not limited to, the inability to walk without the use of a walker, two crutches or two canes, the inability to walk a block at a reasonable pace on rough or uneven surfaces, the inability to use standard public transportation, the inability to carry out routine ambulatory activities, such as shopping and banking, and the inability to climb a few steps at a reasonable pace with the use of a single hand rail. The ability to walk independently about one's home without the use of assistive devices does not, in and of itself, constitute effective ambulation.
c. What we mean by inability to perform fine and gross movements effectively. Inability to perform fine and gross movements effectively means an extreme loss of function of both upper extremities; i.e., an impairment(s) that interferes very seriously with the individual's ability to independently initiate, sustain, or complete activities. To use their upper extremities effectively, individuals must be capable of sustaining such functions as reaching, pushing, pulling, grasping, and fingering to be able to carry out activities of daily living. Therefore, examples of inability to perform fine and gross movements effectively include, but are not limited to, the inability to prepare a simple meal and feed oneself, the inability to take care of personal hygiene, the inability to sort and handle papers or files, and the inability to place files in a file cabinet at or above waist level.
d. Pain or other symptoms. Pain or other symptoms may be an important factor contributing to functional loss. In order for pain or other symptoms to be found to affect an individual's ability to perform basic work activities, medical signs or laboratory findings must show the existence of a medically determinable impairment(s) that could reasonably be expected to produce the pain or other symptoms. The musculoskeletal listings that include pain or other symptoms among their criteria also include criteria for limitations in functioning as a result of the listed impairment, including limitations caused by pain. It is, therefore, important to evaluate the intensity and persistence of such pain or other symptoms carefully in order to determine their impact on the individual's functioning under these listings. See also §§ (f) and of this part, and §§ (f) and of part of this chapter.
C. Diagnosis and Evaluation
1. General. Diagnosis and evaluation of musculoskeletal impairments should be supported, as applicable, by detailed descriptions of the joints, including ranges of motion, condition of the musculature (e.g., weakness, atrophy), sensory or reflex changes, circulatory deficits, and laboratory findings, including findings on x-ray or other appropriate medically acceptable imaging. Medically acceptable imaging includes, but is not limited to, x-ray imaging, computerized axial tomography (CAT scan) or magnetic resonance imaging (MRI), with or without contrast material, myelography, and radionuclear bone scans. “Appropriate” means that the technique used is the proper one to support the evaluation and diagnosis of the impairment.
2. Purchase of certain medically acceptable imaging. While any appropriate medically acceptable imaging is useful in establishing the diagnosis of musculoskeletal impairments, some tests, such as CAT scans and MRIs, are quite expensive, and we will not routinely purchase them. Some, such as myelograms, are invasive and may involve significant risk. We will not order such tests. However, when the results of any of these tests are part of the existing evidence in the case record we will consider them together with the other relevant evidence.
3. Consideration of electrodiagnostic procedures. Electrodiagnostic procedures may be useful in establishing the clinical diagnosis, but do not constitute alternative criteria to the requirements of
D. The physical examination must include a detailed description of the rheumatological, orthopedic, neurological, and other findings appropriate to the specific impairment being evaluated. These physical findings must be determined on the basis of objective observation during the examination and not simply a report of the individual's allegation; e.g., “He says his leg is weak, numb.” Alternative testing methods should be used to verify the abnormal findings; e.g., a seated straight-leg raising test in addition to a supine straight-leg raising test. Because abnormal physical findings may be intermittent, their presence over a period of time must be established by a record of ongoing management and evaluation. Care must be taken to ascertain that the reported examination findings are consistent with the individual's daily activities.
E. Examination of the Spine
1. General. Examination of the spine should include a detailed description of gait, range of motion of the spine given quantitatively in degrees from the vertical position (zero degrees) or, for straight-leg raising from the sitting and supine position (zero degrees), any other appropriate tension signs, motor and sensory abnormalities, muscle spasm, when present, and deep tendon reflexes. Observations of the individual during the examination should be reported; e.g., how he or she gets on and off the examination table. Inability to walk on the heels or toes, to squat, or to arise from a squatting position, when appropriate, may be considered evidence of significant motor loss. However, a report of atrophy is not acceptable as evidence of significant motor loss without circumferential measurements of both thighs and lower legs, or both upper and lower arms, as appropriate, at a stated point above and below the knee or elbow given in inches or centimeters. Additionally, a report of atrophy should be accompanied by measurement of the strength of the muscle(s) in question generally based on a grading system of 0 to 5, with 0 being complete loss of strength and 5 being maximum strength. A specific description of atrophy of hand muscles is acceptable without measurements of atrophy but should include measurements of grip and pinch strength.
2. When neurological abnormalities persist. Neurological abnormalities may not completely subside after treatment or with the passage of time. Therefore, residual neurological abnormalities that persist after it has been determined clinically or by direct surgical or other observation that the ongoing or progressive condition is no longer present will not satisfy the required findings in More serious neurological deficits (paraparesis, paraplegia) are to be evaluated under the criteria in ff.
F. Major joints refers to the major peripheral joints, which are the hip, knee, shoulder, elbow, wrist-hand, and ankle-foot, as opposed to other peripheral joints (e.g., the joints of the hand or forefoot) or axial joints (i.e., the joints of the spine.) The wrist and hand are considered together as one major joint, as are the ankle and foot. Since only the ankle joint, which consists of the juncture of the bones of the lower leg (tibia and fibula) with the hindfoot (tarsal bones), but not the forefoot, is crucial to weight bearing, the ankle and foot are considered separately in evaluating weight bearing.
G. Measurements of joint motion are based on the techniques described in the chapter on the extremities, spine, and pelvis in the current edition of the “Guides to the Evaluation of Permanent Impairment” published by the American Medical Association.
H. Documentation
1. General. Musculoskeletal impairments frequently improve with time or respond to treatment. Therefore, a longitudinal clinical record is generally important for the assessment of severity and expected duration of an impairment unless the claim can be decided favorably on the basis of the current evidence.
2. Documentation of medically prescribed treatment and response. Many individuals, especially those who have listing-level impairments, will have received the benefit of medically prescribed treatment. Whenever evidence of such treatment is available it must be considered.
3. When there is no record of ongoing treatment. Some individuals will not have received ongoing treatment or have an ongoing relationship with the medical community despite the existence of a severe impairment(s). In such cases, evaluation will be made on the basis of the current objective medical evidence and other available evidence, taking into consideration the individual's medical history, symptoms, and medical source opinions. Even though an individual who does not receive treatment may not be able to show an impairment that meets the criteria of one of the musculoskeletal listings, the individual may have an impairment(s) equivalent in severity to one of the listed impairments or be disabled based on consideration of his or her residual functional capacity (RFC) and age, education and work experience.
4. Evaluation when the criteria of a musculoskeletal listing are not met. These listings are only examples of common musculoskeletal disorders that are severe enough to prevent a person from engaging in gainful activity. Therefore, in any case in which an individual has a medically determinable impairment that is not listed, an impairment that does not meet the requirements of a listing, or a combination of impairments no one of which meets the requirements of a listing, we will consider medical equivalence. (See §§ and ) Individuals who have an impairment(s) with a level of severity that does not meet or equal the criteria of the musculoskeletal listings may or may not have the RFC that would enable them to engage in substantial gainful activity. Evaluation of the impairment(s) of these individuals should proceed through the final steps of the sequential evaluation process in §§ and (or, as appropriate, the steps in the medical improvement review standard in §§ and ).
I. Effects of Treatment
1. General. Treatments for musculoskeletal disorders may have beneficial effects or adverse side effects. Therefore, medical treatment (including surgical treatment) must be considered in terms of its effectiveness in ameliorating the signs, symptoms, and laboratory abnormalities of the disorder, and in terms of any side effects that may further limit the individual.
2. Response to treatment. Response to treatment and adverse consequences of treatment may vary widely. For example, a pain medication may relieve an individual's pain completely, partially, or not at all. It may also result in adverse effects, e.g., drowsiness, dizziness, or disorientation, that compromise the individual's ability to function. Therefore, each case must be considered on an individual basis, and include consideration of the effects of treatment on the individual's ability to function.
3. Documentation. A specific description of the drugs or treatment given (including surgery), dosage, frequency of administration, and a description of the complications or response to treatment should be obtained. The effects of treatment may be temporary or long-term. As such, the finding regarding the impact of treatment must be based on a sufficient period of treatment to permit proper consideration or judgment about future functioning.
J. Orthotic, Prosthetic, or Assistive Devices
1. General. Consistent with clinical practice, individuals with musculoskeletal impairments may be examined with and without the use of any orthotic, prosthetic, or assistive devices as explained in this section.
2. Orthotic devices. Examination should be with the orthotic device in place and should include an evaluation of the individual's maximum ability to function effectively with the orthosis. It is unnecessary to routinely evaluate the individual's ability to function without the orthosis in place. If the individual has difficulty with, or is unable to use, the orthotic device, the medical basis for the difficulty should be documented. In such cases, if the impairment involves a lower extremity or extremities, the examination should include information on the individual's ability to ambulate effectively without the device in place unless contraindicated by the medical judgment of a physician who has treated or examined the individual.
3. Prosthetic devices. Examination should be with the prosthetic device in place. In amputations involving a lower extremity or extremities, it is unnecessary to evaluate the individual's ability to walk without the prosthesis in place. However, the individual's medical ability to use a prosthesis to ambulate effectively, as defined in B2b, should be evaluated. The condition of the stump should be evaluated without the prosthesis in place.
4. Hand-held assistive devices. When an individual with an impairment involving a lower extremity or extremities uses a hand-held assistive device, such as a cane, crutch or walker, examination should be with and without the use of the assistive device unless contraindicated by the medical judgment of a physician who has treated or examined the individual. The individual's ability to ambulate with and without the device provides information as to whether, or the extent to which, the individual is able to ambulate without assistance. The medical basis for the use of any assistive device (e.g., instability, weakness) should be documented. The requirement to use a hand-held assistive device may also impact on the individual's functional capacity by virtue of the fact that one or both upper extremities are not available for such activities as lifting, carrying, pushing, and pulling.
K. Disorders of the spine, listed in , result in limitations because of distortion of the bony and ligamentous architecture of the spine and associated impingement on nerve roots (including the cauda equina) or spinal cord. Such impingement on nerve tissue may result from a herniated nucleus pulposus, spinal stenosis, arachnoiditis, or other miscellaneous conditions.
1. Herniated nucleus pulposus is a disorder frequently associated with the impingement of a nerve root. Nerve root compression results in a specific neuro-anatomic distribution of symptoms and signs depending upon the nerve root(s) compromised.
2. Spinal Arachnoiditis
a. General. Spinal arachnoiditis is a condition characterized by adhesive thickening of the arachnoid which may cause intermittent ill-defined burning pain and sensory dysesthesia, and may cause neurogenic bladder or bowel incontinence when the cauda equina is involved.
b. Documentation. Although the cause of spinal arachnoiditis is not always clear, it may be associated with chronic compression or irritation of nerve roots (including the cauda equina) or the spinal cord. For example, there may be evidence of spinal stenosis, or a history of spinal trauma or meningitis. Diagnosis must be confirmed at the time of surgery by gross description, microscopic examination of biopsied tissue, or by findings on appropriate medically acceptable imaging. Arachnoiditis is sometimes used as a diagnosis when such a diagnosis is unsupported by clinical or laboratory findings. Therefore, care must be taken to ensure that the diagnosis is documented as described in B. Individuals with arachnoiditis, particularly when it involves the lumbosacral spine, are generally unable to sustain any given position or posture for more than a short period of time due to pain.
3. Lumbar spinal stenosis is a condition that may occur in association with degenerative processes, or as a result of a congenital anomaly or trauma, or in association with Paget's disease of the bone. Pseudoclaudication, which may result from lumbar spinal stenosis, is manifested as pain and weakness, and may impair ambulation. Symptoms are usually bilateral, in the low back, buttocks, or thighs, although some individuals may experience only leg pain and, in a few cases, the leg pain may be unilateral. The pain generally does not follow a particular neuro-anatomical distribution, i.e., it is distinctly different from the radicular type of pain seen with a herniated intervertebral disc, is often of a dull, aching quality, which may be described as “discomfort” or an “unpleasant sensation,” or may be of even greater severity, usually in the low back and radiating into the buttocks region bilaterally. The pain is provoked by extension of the spine, as in walking or merely standing, but is reduced by leaning forward. The distance the individual has to walk before the pain comes on may vary. Pseudoclaudication differs from peripheral vascular claudication in several ways. Pedal pulses and Doppler examinations are unaffected by pseudoclaudication. Leg pain resulting from peripheral vascular claudication involves the calves, and the leg pain in vascular claudication is ordinarily more severe than any back pain that may also be present. An individual with vascular claudication will experience pain after walking the same distance time after time, and the pain will be relieved quickly when walking stops.
4. Other miscellaneous conditions that may cause weakness of the lower extremities, sensory changes, areflexia, trophic ulceration, bladder or bowel incontinence, and that should be evaluated under include, but are not limited to, osteoarthritis, degenerative disc disease, facet arthritis, and vertebral fracture. Disorders such as spinal dysrhaphism (e.g., spina bifida), diastematomyelia, and tethered cord syndrome may also cause such abnormalities. In these cases, there may be gait difficulty and deformity of the lower extremities based on neurological abnormalities, and the neurological effects are to be evaluated under the criteria in ff.
L. Abnormal curvatures of the spine. Abnormal curvatures of the spine (specifically, scoliosis, kyphosis and kyphoscoliosis) can result in impaired ambulation, but may also adversely affect functioning in body systems other than the musculoskeletal system. For example, an individual's ability to breathe may be affected; there may be cardiac difficulties (e.g., impaired myocardial function); or there may be disfigurement resulting in withdrawal or isolation. When there is impaired ambulation, evaluation of equivalence may be made by reference to A. When the abnormal curvature of the spine results in symptoms related to fixation of the dorsolumbar or cervical spine, evaluation of equivalence may be made by reference to C. When there is respiratory or cardiac involvement or an associated mental disorder, evaluation may be made under ff, ff, or ff, as appropriate. Other consequences should be evaluated according to the listing for the affected body system.
M. Under continuing surgical management, as used in and , refers to surgical procedures and any other associated treatments related to the efforts directed toward the salvage or restoration of functional use of the affected part. It may include such factors as post-surgical procedures, surgical complications, infections, or other medical complications, related illnesses, or related treatments that delay the individual's attainment of maximum benefit from therapy. When burns are not under continuing surgical management, see F.
N. After maximum benefit from therapy has been achieved in situations involving fractures of an upper extremity (), or soft tissue injuries (), i.e., there have been no significant changes in physical findings or on appropriate medically acceptable imaging for any 6-month period after the last definitive surgical procedure or other medical intervention, evaluation must be made on the basis of the demonstrable residuals, if any. A finding that or is met must be based on a consideration of the symptoms, signs, and laboratory findings associated with recent or anticipated surgical procedures and the resulting recuperative periods, including any related medical complications, such as infections, illnesses, and therapies which impede or delay the efforts toward restoration of function. Generally, when there has been no surgical or medical intervention for 6 months after the last definitive surgical procedure, it can be concluded that maximum therapeutic benefit has been reached. Evaluation at this point must be made on the basis of the demonstrable residual limitations, if any, considering the individual's impairment-related symptoms, signs, and laboratory findings, any residual symptoms, signs, and laboratory findings associated with such surgeries, complications, and recuperative periods, and other relevant evidence.
O. Major function of the face and head, for purposes of listing , relates to impact on any or all of the activities involving vision, hearing, speech, mastication, and the initiation of the digestive process.
P. When surgical procedures have been performed, documentation should include a copy of the operative notes and available pathology reports.
Q. Effects of obesity. Obesity is a medically determinable impairment that is often associated with disturbance of the musculoskeletal system, and disturbance of this system can be a major cause of disability in individuals with obesity. The combined effects of obesity with musculoskeletal impairments can be greater than the effects of each of the impairments considered separately. Therefore, when determining whether an individual with obesity has a listing-level impairment or combination of impairments, and when assessing a claim at other steps of the sequential evaluation process, including when assessing an individual's residual functional capacity, adjudicators must consider any additional and cumulative effects of obesity.
Category of Impairments, Musculoskeletal
Major dysfunction of a joint(s) (due to any cause): Characterized by gross anatomical deformity (e.g., subluxation, contracture, bony or fibrous ankylosis, instability) and chronic joint pain and stiffness with signs of limitation of motion or other abnormal motion of the affected joint(s), and findings on appropriate medically acceptable imaging of joint space narrowing, bony destruction, or ankylosis of the affected joint(s). With:
A. Involvement of one major peripheral weight-bearing joint (i.e., hip, knee, or ankle), resulting in inability to ambulate effectively, as defined in B2b;
or
B. Involvement of one major peripheral joint in each upper extremity (i.e., shoulder, elbow, or wrist-hand), resulting in inability to perform fine and gross movements effectively, as defined in B2c.
Reconstructive surgery or surgical arthrodesis of a major weight-bearing joint, with inability to ambulate effectively, as defined in B2b, and return to effective ambulation did not occur, or is not expected to occur, within 12 months of onset.
Disorders of the spine (e.g., herniated nucleus pulposus, spinal arachnoiditis, spinal stenosis, osteoarthritis, degenerative disc disease, facet arthritis, vertebral fracture), resulting in compromise of a nerve root (including the cauda equina) or the spinal cord. With:
A. Evidence of nerve root compression characterized by neuro-anatomic distribution of pain, limitation of motion of the spine, motor loss (atrophy with associated muscle weakness or muscle weakness) accompanied by sensory or reflex loss and, if there is involvement of the lower back, positive straight-leg raising test (sitting and supine);
or
B. Spinal arachnoiditis, confirmed by an operative note or pathology report of tissue biopsy, or by appropriate medically acceptable imaging, manifested by severe burning or painful dysesthesia, resulting in the need for changes in position or posture more than once every 2 hours;
or
C. Lumbar spinal stenosis resulting in pseudoclaudication, established by findings on appropriate medically acceptable imaging, manifested by chronic nonradicular pain and weakness, and resulting in inability to ambulate effectively, as defined in B2b.
Amputation (due to any cause).
A. Both hands; or
or
B. One or both lower extremities at or above the tarsal region, with stump complications resulting in medical inability to use a prosthetic device to ambulate effectively, as defined in B2b, which have lasted or are expected to last for at least 12 months;
or
C. One hand and one lower extremity at or above the tarsal region, with inability to ambulate effectively, as defined in B2b; OR
D. Hemipelvectomy or hip disarticulation.
Fracture of the femur, tibia, pelvis, or one or more of the tarsal bones. With:
A. Solid union not evident on appropriate medically acceptable imaging and not clinically solid;
and
B. Inability to ambulate effectively, as defined in B2b, and return to effective ambulation did not occur or is not expected to occur within 12 months of onset.
Fracture of an upper extremity with nonunion of a fracture of the shaft of the humerus, radius, or ulna, under continuing surgical management, as defined in M, directed toward restoration of functional use of the extremity, and such function was not restored or expected to be restored within 12 months of onset.
Soft tissue injury (e.g., burns) of an upper or lower extremity, trunk, or face and head, under continuing surgical management, as defined in M, directed toward the salvage or restoration of major function, and such major function was not restored or expected to be restored within 12 months of onset. Major function of the face and head is described in O.
Special Senses and Speech
A. How do we evaluate visual disorders?
1. What are visual disorders? Visual disorders are abnormalities of the eye, the optic nerve, the optic tracts, or the brain that may cause a loss of visual acuity or visual fields. A loss of visual acuity limits your ability to distinguish detail, read, or do fine work. A loss of visual fields limits your ability to perceive visual stimuli in the peripheral extent of vision.
2. How do we define statutory blindness? Statutory blindness is blindness as defined in sections (i)(1) and (a)(2) of the Social Security Act (Act).
a. The Act defines blindness as central visual acuity of 20/ or less in the better eye with the use of a correcting lens. We use your best-corrected central visual acuity for distance in the better eye when we determine if this definition is met. (For visual acuity testing requirements, see A5.)
b. The Act also provides that an eye that has a visual field limitation such that the widest diameter of the visual field subtends an angle no greater than 20 degrees is considered as having a central visual acuity of 20/ or less. (For visual field testing requirements, see A6.)
c. You have statutory blindness only if your visual disorder meets the criteria of or A. You do not have statutory blindness if your visual disorder medically equals the criteria of or A or meets or medically equals the criteria of B, C, A, or B because your disability is based on criteria other than those in the statutory definition of blindness.
3. What evidence do we need to establish statutory blindness under title XVI? To establish that you have statutory blindness under title XVI, we need evidence showing only that your central visual acuity in your better eye or your visual field in your better eye meets the criteria in A2, provided that those measurements are consistent with the other evidence in your case record. We do not need documentation of the cause of your blindness. Also, there is no duration requirement for statutory blindness under title XVI (see §§ and of this chapter).
4. What evidence do we need to evaluate visual disorders, including those that result in statutory blindness under title II? To evaluate your visual disorder, we usually need a report of an eye examination that includes measurements of your best-corrected central visual acuity (see A5) or the extent of your visual fields (see A6), as appropriate. If you have visual acuity or visual field loss, we need documentation of the cause of the loss. A standard eye examination will usually indicate the cause of any visual acuity loss. A standard eye examination can also indicate the cause of some types of visual field deficits. Some disorders, such as cortical visual disorders, may result in abnormalities that do not appear on a standard eye examination. If the standard eye examination does not indicate the cause of your vision loss, we will request the information used to establish the presence of your visual disorder. If your visual disorder does not satisfy the criteria in , , or , we will request a description of how your visual disorder affects your ability to function.
5. How do we measure your best-corrected central visual acuity?
a. Visual acuity testing. When we need to measure your best-corrected central visual acuity (your optimal visual acuity attainable with the use of a corrective lens), we use visual acuity testing for distance that was carried out using Snellen methodology or any other testing methodology that is comparable to Snellen methodology.
(i) Your best-corrected central visual acuity for distance is usually measured by determining what you can see from 20 feet. If your visual acuity is measured for a distance other than 20 feet, we will convert it to a foot measurement. For example, if your visual acuity is measured at 10 feet and is reported as 10/40, we will convert this measurement to 20/
(ii) A visual acuity recorded as CF (counts fingers), HM (hand motion only), LP or LPO (light perception or light perception only), or NLP (no light perception) indicates that no optical correction will improve your visual acuity. If your central visual acuity in an eye is recorded as CF, HM, LP or LPO, or NLP, we will determine that your best-corrected central visual acuity is 20/ or less in that eye.
(iii) We will not use the results of pinhole testing or automated refraction acuity to determine your best-corrected central visual acuity. These tests provide an estimate of potential visual acuity but not an actual measurement of your best-corrected central visual acuity.
b. Other test charts. Most test charts that use Snellen methodology do not have lines that measure visual acuity between 20/ and 20/ Some test charts, such as the Bailey-Lovie or the Early Treatment Diabetic Retinopathy Study (ETDRS), used mostly in research settings, have such lines. If your visual acuity is measured with one of these charts, and you cannot read any of the letters on the 20/ line, we will determine that you have statutory blindness based on a visual acuity of 20/ or less. For example, if your best-corrected central visual acuity for distance in the better eye is 20/ using an ETDRS chart, we will find that you have statutory blindness. Regardless of the type of test chart used, you do not have statutory blindness if you can read at least one letter on the 20/ line. For example, if your best-corrected central visual acuity for distance in the better eye is 20/ + 1 using an ETDRS chart, we will find that you do not have statutory blindness because you are able to read one letter on the 20/ line.
c. Testing using a specialized lens. In some instances, you may have visual acuity testing performed using specialized lens, such as a contact lens. We will use the visual acuity measurements obtained with a specialized lens only if you have demonstrated the ability to use the specialized lens on a sustained basis. We will not use visual acuity measurements obtained with telescopic lenses.
d. Cycloplegic refraction is an examination of the eye performed after administering cycloplegic eye drops capable of relaxing the ability of the pupil to become smaller and temporarily paralyzing the focusing muscles. If your case record contains the results of cycloplegic refraction, we may use the results to determine your best-corrected central visual acuity. We will not purchase cycloplegic refraction.
e. Visual evoked response (VER) testing measures your response to visual events and can often detect dysfunction that is undetectable through other types of examinations. If you have an absent response to VER testing in your better eye, we will determine that your best-corrected central visual acuity is 20/ or less in that eye and that your visual acuity loss satisfies the criterion in when these test results are consistent with the other evidence in your case record. If you have a positive response to VER testing in an eye, we will not use that result to determine your best-corrected central visual acuity in that eye.
6. How do we measure your visual fields?
a. General. We generally need visual field testing when you have a visual disorder that could result in visual field loss, such as glaucoma, retinitis pigmentosa, or optic neuropathy, or when you display behaviors that suggest a visual field loss. When we need to measure the extent of your visual field loss, we use visual field testing (also referred to as perimetry) carried out using automated static threshold perimetry performed on an acceptable perimeter. (For perimeter requirements, see A9.)
b. Automated static threshold perimetry requirements.
(i) The test must use a white size III Goldmann stimulus and a apostilb (asb) white background (or a 10 candela per square meter (cd/m2) white background). The stimuli test locations must be no more than 6 degrees apart horizontally or vertically. Measurements must be reported on standard charts and include a description of the size and intensity of the test stimulus.
(ii) We measure the extent of your visual field loss by determining the portion of the visual field in which you can see a white III4e stimulus. The “III” refers to the standard Goldmann test stimulus size III (4 mm2), and the “4e” refers to the standard Goldmann intensity filter (0 decibel (dB) attenuation, which allows presentation of the maximum luminance) used to determine the intensity of the stimulus.
(iii) In automated static threshold perimetry, the intensity of the stimulus varies. The intensity of the stimulus is expressed in decibels (dB). A perimeter's maximum stimulus luminance is usually assigned the value 0 dB. We need to determine the dB level that corresponds to a 4e intensity for the particular perimeter being used. We will then use the dB printout to determine which points you see at a 4e intensity level (a “seeing point”). For example:
A. When the maximum stimulus luminance (0 dB stimulus) on an acceptable perimeter is 10, asb, a 10 dB stimulus is equivalent to a 4e stimulus. Any point you see at 10 dB or greater is a seeing point.
B. When the maximum stimulus luminance (0 dB stimulus) on an acceptable perimeter is 4, asb, a 6 dB stimulus is equivalent to a 4e stimulus. Any point you see at 6 dB or greater is a seeing point.
C. When the maximum stimulus luminance (0 dB stimulus) on an acceptable perimeter is 1, asb, a 0 dB stimulus is equivalent to a 4e stimulus. Any point you see at 0 dB or greater is a seeing point.
c. Evaluation under A. To determine statutory blindness based on visual field loss in your better eye (A), we need the results of a visual field test that measures the central 24 to 30 degrees of your visual field; that is, the area measuring 24 to 30 degrees from the point of fixation. Acceptable tests include the Humphrey Field Analyzer (HFA) , HFA , and Octopus
d. Evaluation under B. To determine whether your visual field loss meets listing B, we use the mean deviation or defect (MD) from acceptable automated static threshold perimetry that measures the central 30 degrees of the visual field. MD is the average sensitivity deviation from normal values for all measured visual field locations. When using results from HFA tests, which report the MD as a negative number, we use the absolute value of the MD to determine whether your visual field loss meets listing B. We cannot use tests that do not measure the central 30 degrees of the visual field, such as the HFA , to determine if your impairment meets or medically equals B.
e. Other types of perimetry. If the evidence in your case contains visual field measurements obtained using manual or automated kinetic perimetry, such as Goldmann perimetry or the HFA “SSA Test Kinetic,” we can generally use these results if the kinetic test was performed using a white III4e stimulus projected on a white asb (10 cd/m2) background. Automated kinetic perimetry, such as the HFA “SSA Test Kinetic,” does not detect limitations in the central visual field because testing along a meridian stops when you see the stimulus. If your visual disorder has progressed to the point at which it is likely to result in a significant limitation in the central visual field, such as a scotoma (see A6h), we will not use automated kinetic perimetry to determine the extent of your visual field loss. Instead, we will determine the extent of your visual field loss using automated static threshold perimetry or manual kinetic perimetry.
f. Screening tests. We will not use the results of visual field screening tests, such as confrontation tests, tangent screen tests, or automated static screening tests, to determine that your impairment meets or medically equals a listing or to evaluate your residual functional capacity. We can consider normal results from visual field screening tests to determine whether your visual disorder is severe when these test results are consistent with the other evidence in your case record. (See §§ (c), , (c), and of this chapter.) We will not consider normal test results to be consistent with the other evidence if the clinical findings indicate that your visual disorder has progressed to the point that it is likely to cause visual field loss, or you have a history of an operative procedure for retinal detachment.
g. Use of corrective lenses. You must not wear eyeglasses during visual field testing because they limit your field of vision. You may wear contact lenses to correct your visual acuity during the visual field test to obtain the most accurate visual field measurements. For this single purpose, you do not need to demonstrate that you have the ability to use the contact lenses on a sustained basis.
h. Scotoma. A scotoma is a field defect or non-seeing area (also referred to as a “blind spot”) in the visual field surrounded by a normal field or seeing area. When we measure your visual field, we subtract the length of any scotoma, other than the normal blind spot, from the overall length of any diameter on which it falls.
7. How do we determine your visual acuity efficiency, visual field efficiency, and visual efficiency?
a. General. Visual efficiency, a calculated value of your remaining visual function, is the combination of your visual acuity efficiency and your visual field efficiency expressed as a percentage.
b. Visual acuity efficiency. Visual acuity efficiency is a percentage that corresponds to the best-corrected central visual acuity for distance in your better eye. See Table 1.
| Snellen best-corrected central visual acuity for distance | Visual acuity efficiency (%)(A) | |
|---|---|---|
| English | Metric | |
| 20/16 | 6/5 | |
| 20/20 | 6/6 | |
| 20/25 | 6/ | 95 |
| 20/30 | 6/9 | 90 |
| 20/40 | 6/12 | 85 |
| 20/50 | 6/15 | 75 |
| 20/60 | 6/18 | 70 |
| 20/70 | 6/21 | 65 |
| 20/80 | 6/24 | 60 |
| 20/ | 6/30 | 50 |
c. Visual field efficiency. Visual field efficiency is a percentage that corresponds to the visual field in your better eye. Under C, we require kinetic perimetry to determine your visual field efficiency percentage. We calculate the visual field efficiency percentage by adding the number of degrees you see along the eight principal meridians found on a visual field chart (0, 45, 90, , , , , and ) in your better eye and dividing by 5. For example, in Figure 1:
A. The diagram of the left eye illustrates a visual field, as measured with a III4e stimulus, contracted to 30 degrees in two meridians ( and ) and to 20 degrees in the remaining six meridians. The visual efficiency percentage of this field is: ((2 × 30) + (6 × 20)) ÷ 5 = 36 percent.
B. The diagram of the right eye illustrates the extent of a normal visual field as measured with a III4e stimulus. The sum of the eight principal meridians of this field is degrees. The visual efficiency percentage of this field is ÷ 5 = percent.
d. Visual efficiency. Under A, we calculate the visual efficiency percentage by multiplying your visual acuity efficiency percentage (see A7b) by your visual field efficiency percentage (see A7c) and dividing by For example, if your visual acuity efficiency percentage is 75 and your visual field efficiency percentage is 36, your visual efficiency percentage is: (75 × 36) ÷ = 27 percent.
8. How do we determine your visual acuity impairment value, visual field impairment value, and visual impairment value?
a. General. Visual impairment value, a calculated value of your loss of visual function, is the combination of your visual acuity impairment value and your visual field impairment value.
b. Visual acuity impairment value. Your visual acuity impairment value corresponds to the best-corrected central visual acuity for distance in your better eye. See Table 2.
| Snellen best-corrected central visual acuity for distance | Visual acuityimpairment value (B) | |
| English | Metric | |
| 20/16 | 6/5 | |
| 20/20 | 6/6 | |
| 20/25 | 6/ | |
| 20/30 | 6/9 | |
| 20/40 | 6/12 | |
| 20/50 | 6/15 | |
| 20/60 | 6/18 | |
| 20/70 | 6/21 | |
| 20/80 | 6/24 | |
| 20/ | 6/30 |
c. Visual field impairment value. Your visual field impairment value corresponds to the visual field in your better eye. Using the MD from acceptable automated static threshold perimetry, we calculate the visual field impairment value by dividing the absolute value of the MD by For example, if your MD on an HFA is −16, your visual field impairment value is: −16| ÷ 22 =
d. Visual impairment value. Under B, we calculate the visual impairment value by adding your visual acuity impairment value (see A8b) and your visual field impairment value (see A8c). For example, if your visual acuity impairment value is and your visual field impairment value is , your visual impairment value is: + =
9. What are our requirements for an acceptable perimeter? We will use results from automated static threshold perimetry performed on a perimeter that:
a. Uses optical projection to generate the test stimuli.
b. Has an internal normative database for automatically comparing your performance with that of the general population.
c. Has a statistical analysis package that is able to calculate visual field indices, particularly MD.
d. Demonstrates the ability to correctly detect visual field loss and correctly identify normal visual fields.
e. Demonstrates good test-retest reliability.
f. Has undergone clinical validation studies by three or more independent laboratories with results published in peer-reviewed ophthalmic journals.
B. How do we evaluate hearing loss?
1. What evidence do we need?
a. We need evidence showing that you have a medically determinable impairment that causes your hearing loss and audiometric measurements of the severity of your hearing loss. We generally require both an otologic examination and audiometric testing to establish that you have a medically determinable impairment that causes your hearing loss. You should have this audiometric testing within 2 months of the otologic examination. Once we have evidence that you have a medically determinable impairment, we can use the results of later audiometric testing to assess the severity of your hearing loss without another otologic examination. We will consider your test scores together with any other relevant information we have about your hearing, including information from outside of the test setting.
b. The otologic examination must be performed by a licensed physician (medical or osteopathic doctor) or audiologist. It must include your medical history, your description of how your hearing loss affects you, and the physician's or audiologist's description of the appearance of the external ears (pinnae and external ear canals), evaluation of the tympanic membranes, and assessment of any middle ear abnormalities.
c. Audiometric testing must be performed by, or under the directsupervision of, a licensed audiologist or an otolaryngologist.
2. What audiometric testing do we need when you do not have a cochlear implant?
a. We generally need pure tone air conduction and bone conduction testing, speech reception threshold (SRT) testing (also referred to as “spondee threshold” or “ST” testing), and word recognition testing (also referred to as “word discrimination” or “speech discrimination” testing). This testing must be conducted in a sound-treated booth or room and must be in accordance with the most recently published standards of the American National Standards Institute (ANSI). Each ear must be tested separately.
b. You must not wear hearing aids during the testing. Additionally, a person described in B1c must perform an otoscopic examination immediately before the audiometric testing. (An otoscopic examination provides a description of the appearance of your external ear canals and an evaluation of the tympanic membranes. In these rules, we use the term to include otoscopic examinations performed by physicians and otoscopic inspections performed by audiologists and others.) The otoscopic examination must show that there are no conditions that would prevent valid audiometric testing, such as fluid in the ear, ear infection, or obstruction in an ear canal. The person performing the test should also report on any other factors, such as your cooperation with the test, that can affect the interpretation of the test results.
c. To determine whether your hearing loss meets the air and bone conduction criteria in A, we will average your air and bone conduction hearing thresholds at , , and Hertz (Hz). If you do not have a response at a particular frequency, we will use a threshold of 5 decibels (dB) over the limit of the audiometer.
d. The SRT is the minimum dB level required for you to recognize 50 percent of the words on a standard list of spondee words. (Spondee words are two-syllable words that have equal stress on each syllable.) The SRT is usually within 10 dB of the average pure tone air conduction hearing thresholds at , , and Hz. If the SRT is not within 10 dB of the average pure tone air conduction threshold, the reason for the discrepancy must be documented. If we cannot determine that there is a medical basis for the discrepancy, we will not use the results of the testing to determine whether your hearing loss meets a listing.
e. Word recognition testing determines your ability to recognize a standardized list of phonetically balanced monosyllabic words in the absence of any visual cues. This testing must be performed in quiet. The list may be recorded or presented live, but in either case the words should be presented at a level of amplification that will measure your maximum ability to discriminate words, usually 35 to 40 dB above your SRT. However, the amplification level used in the testing must be medically appropriate, and you must be able to tolerate it. If you cannot be tested at 35 to 40 dB above your SRT, the person who performs the test should report your word recognition testing score at your highest comfortable level of amplification.
3. What audiometric testing do we need when you have a cochlear implant?
a. If you have a cochlear implant, we will consider you to be disabled until 1 year after initial implantation.
b. After that period, we need word recognition testing performed with any version of the Hearing in Noise Test (HINT) to determine whether your impairment meets B. This testing must be conducted in quiet in a sound field. Your implant must be functioning properly and adjusted to your normal settings. The sentences should be presented at 60 dB HL (Hearing Level) and without any visual cues.
4. How do we evaluate your word recognition ability if you are not fluent in English?
If you are not fluent in English, you should have word recognition testing using an appropriate word list for the language in which you are most fluent. The person conducting the test should be fluent in the language used for the test. If there is no appropriate word list or no person who is fluent in the language and qualified to perform the test, it may not be possible to measure your word recognition ability. If your word recognition ability cannot be measured, your hearing loss cannot meet B or B. Instead, we will consider the facts of your case to determine whether you have difficulty understanding words in the language in which you are most fluent, and if so, whether that degree of difficulty medically equals B or B. For example, we will consider how you interact with family members, interpreters, and other persons who speak the language in which you are most fluent.
C. How do we evaluate vertigo associated with disturbances of labyrinthine-vestibular function, including Meniere's disease?
1. These disturbances of balance are characterized by an hallucination of motion or loss of position sense and a sensation of dizziness which may be constant or may occur in paroxysmal attacks. Nausea, vomiting, ataxia, and incapacitation are frequently observed, particularly during the acute attack. It is important to differentiate the report of rotary vertigo from that of “dizziness” which is described as lightheadedness, unsteadiness, confusion, or syncope.
2. Meniere's disease is characterized by paroxysmal attacks of vertigo, tinnitus, and fluctuating hearing loss. Remissions are unpredictable and irregular, but may be longlasting; hence, the severity of impairment is best determined after prolonged observation and serial reexaminations.
3. The diagnosis of a vestibular disorder requires a comprehensive neuro-otolaryngologic examination with a detailed description of the vertiginous episodes, including notation of frequency, severity, and duration of the attacks. Pure tone and speech audiometry with the appropriate special examinations, such as Bekesy audiometry, are necessary. Vestibular functions is assessed by positional and caloric testing, preferably by electronystagmography. When polytomograms, contrast radiography, or other special tests have been performed, copies of the reports of these tests should be obtained in addition to appropriate medically acceptable imaging reports of the skull and temporal bone. Medically acceptable imaging includes, but is not limited to, x-ray imaging, computerized axial tomography (CAT scan) or magnetic resonance imaging (MRI), with or without contrast material, myelography, and radionuclear bone scans. “Appropriate” means that the technique used is the proper one to support the evaluation and diagnosis of the impairment.
D. Loss of speech. In evaluating the loss of speech, the ability to produce speech by any means includes the use of mechanical or electronic devices that improve voice or articulation. Impairments of speech may also be evaluated under the body system for the underlying disorder, such as neurological disorders, ff.
E. How do we evaluate impairments that do not meet one of the special senses and speech listings?
1. These listings are only examples of common special senses and speech disorders that we consider severe enough to prevent an individual from doing any gainful activity. If your impairment(s) does not meet the criteria of any of these listings, we must also consider whether you have an impairment(s) that satisfies the criteria of a listing in another body system.
2. If you have a medically determinable impairment(s) that does not meet a listing, we will determine whether the impairment(s) medically equals a listing. (See §§ and ) If you have an impairment(s) that does not meet or medically equal a listing, you may or may not have the residual functional capacity to engage in substantial gainful activity. Therefore, we proceed to the fourth, and if necessary, the fifth steps of the sequential evaluation process in §§ and When we decide whether you continue to be disabled, we use the rules in §§ , , or a, as appropriate.
Category of Impairments, Special Senses and Speech
Loss of central visual acuity. Remaining vision in the better eye after best correction is 20/ or less.
Contraction of the visual field in the better eye, with:
A. The widest diameter subtending an angle around the point of fixation no greater than 20 degrees.
OR
B. An MD of 22 decibels or greater, determined by automated static threshold perimetry that measures the central 30 degrees of the visual field (see A6d).
OR
C. A visual field efficiency of 20 percent or less, determined by kinetic perimetry (see A7c).
Loss of visual efficiency, or visual impairment, in the better eye:
A. A visual efficiency percentage of 20 or less after best correction (see A7d).
OR
B. A visual impairment value of or greater after best correction (see A8d).
Disturbance of labyrinthine-vestibular function (including Meniere's disease), characterized by a history of frequent attacks of balance disturbance, tinnitus, and progressive loss of hearing. With both A and B:
A. Disturbed function of vestibular labyrinth demonstrated by caloric or other vestibular tests; and
B. Hearing loss established by audiometry.
Loss of speech due to any cause, with inability to produce by any means speech that can be heard, understood, or sustained.
| Snellen | Percentvisual acuity efficiency | |
|---|---|---|
| English | Metric | |
| 20/16 | 6/5 | |
| 20/20 | 6/6 | |
| 20/25 | 6/ | 95 |
| 20/30 | 6/9 | 90 |
| 20/40 | 6/12 | 85 |
| 20/50 | 6/15 | 75 |
| 20/60 | 6/18 | 70 |
| 20/70 | 6/21 | 65 |
| 20/80 | 6/24 | 60 |
| 20/ | 6/30 | 50 |
1. The diagram of the right eye illustrates the extent of a normal visual field as measured with a III4e stimulus. The sum of the eight principal meridians of this field is degrees.
2. The diagram of the left eye illustrates a visual field contracted to 30 degrees in two meridians and to 20 degrees in the remaining six meridians. The percent of visual field efficiency of this field is: (2 × 30) + (6 × 20) = ÷ = or 36 percent visual field efficiency.
Hearing loss not treated with cochlear implantation.
A. An average air conduction hearing threshold of 90 decibels or greater in the better ear and an average bone conduction hearing threshold of 60 decibels or greater in the better ear (see B2c).
OR
B. A word recognition score of 40 percent or less in the better ear determined using a standardized list of phonetically balanced monosyllabic words (see B2e).
Hearing loss treated with cochlear implantation.
A. Consider under a disability for 1 year after initial implantation.
OR
B. If more than 1 year after initial implantation, a word recognition score of 60 percent or less determined using the HINT (see B3b).
Respiratory Disorders
A. Which disorders do we evaluate in this body system?
1. We evaluate respiratory disorders that result in obstruction (difficulty moving air out of the lungs) or restriction (difficulty moving air into the lungs), or that interfere with diffusion (gas exchange) across cell membranes in the lungs. Examples of such disorders and the listings we use to evaluate them include chronic obstructive pulmonary disease (chronic bronchitis and emphysema, ), pulmonary fibrosis and pneumoconiosis (), asthma ( or ), cystic fibrosis (), and bronchiectasis ( or ). We also use listings in this body system to evaluate respiratory failure (D or ), chronic pulmonary hypertension (), and lung transplantation ().
2. We evaluate cancers affecting the respiratory system under the listings in We evaluate the pulmonary effects of neuromuscular and autoimmune disorders under these listings or under the listings in or , respectively.
B. What are the symptoms and signs of respiratory disorders? Symptoms and signs of respiratory disorders include dyspnea (shortness of breath), chest pain, coughing, wheezing, sputum production, hemoptysis (coughing up blood from the respiratory tract), use of accessory muscles of respiration, and tachypnea (rapid rate of breathing).
C. What abbreviations do we use in this body system?
1. ABG means arterial blood gas.
2. BiPAP means bi-level positive airway pressure ventilation.
3. BTPS means body temperature and ambient pressure, saturated with water vapor.
4. CF means cystic fibrosis.
5. CFRD means CF-related diabetes.
6. CFTR means CF transmembrane conductance regulator.
7. CO means carbon monoxide.
8. COPD means chronic obstructive pulmonary disease.
9. DLCO means diffusing capacity of the lungs for carbon monoxide.
FEV1 means forced expiratory volume in the first second of a forced expiratory maneuver.
FVC means forced vital capacity.
L means liter.
mL CO (STPD)/min/mmHg means milliliters of carbon monoxide at standard temperature and pressure, dry, per minute, per millimeter of mercury.
PaO2 means arterial blood partial pressure of oxygen.
PaCO2 means arterial blood partial pressure of carbon dioxide.
SpO2 means percentage of oxygen saturation of blood hemoglobin measured by pulse oximetry.
6MWT means 6-minute walk test.
VI means volume of inhaled gas during a DLCO test.
D. What documentation do we need to evaluate your respiratory disorder?
1. We need medical evidence to document and assess the severity of your respiratory disorder. Medical evidence should include your medical history, physical examination findings, the results of imaging (see D3), pulmonary function tests (see D4), other relevant laboratory tests, and descriptions of any prescribed treatment and your response to it. We may not need all of this evidence depending on your particular respiratory disorder and its effects on you.
2. If you use supplemental oxygen, we still need medical evidence to establish the severity of your respiratory disorder.
3. Imaging refers to medical imaging techniques, such as x-ray and computerized tomography. The imaging must be consistent with the prevailing state of medical knowledge and clinical practice as the proper technique to support the evaluation of the disorder.
4. Pulmonary function tests include spirometry (which measures ventilation of the lungs), DLCO tests (which measure gas diffusion in the lungs), ABG tests (which measure the partial pressure of oxygen, PaO2, and carbon dioxide, PaCO2, in the arterial blood), and pulse oximetry (which measures oxygen saturation, SpO2, of peripheral blood hemoglobin).
E. What is spirometry and what are our requirements for an acceptable test and report?
1. Spirometry, which measures how well you move air into and out of your lungs, involves at least three forced expiratory maneuvers during the same test session. A forced expiratory maneuver is a maximum inhalation followed by a forced maximum exhalation, and measures exhaled volumes of air over time. The volume of air you exhale in the first second of the forced expiratory maneuver is the FEV1. The total volume of air that you exhale during the entire forced expiratory maneuver is the FVC. We use your highest FEV1 value to evaluate your respiratory disorder under A, A, and A, and your highest FVC value to evaluate your respiratory disorder under B, regardless of whether the values are from the same forced expiratory maneuver or different forced expiratory maneuvers.
2. We have the following requirements for spirometry under these listings:
a. You must be medically stable at the time of the test. Examples of when we would not consider you to be medically stable include when you are:
(i) Within 2 weeks of a change in your prescribed respiratory medication.
(ii) Experiencing, or within 30 days of completion of treatment for, a lower respiratory tract infection.
(iii) Experiencing, or within 30 days of completion of treatment for, an acute exacerbation (temporary worsening) of a chronic respiratory disorder. Wheezing by itself does not indicate that you are not medically stable.
(iv) Hospitalized, or within 30 days of a hospital discharge, for an acute myocardial infarction (heart attack).
b. During testing, if your FEV1 is less than 70 percent of your predicted normal value, we require repeat spirometry after inhalation of a bronchodilator to evaluate your respiratory disorder under these listings, unless it is medically contraindicated. If you used a bronchodilator before the test and your FEV1 is less than 70 percent of your predicted normal value, we still require repeat spirometry after inhalation of a bronchodilator unless the supervising physician determines that it is not safe for you to take a bronchodilator again (in which case we may need to reschedule the test). If you do not have post-bronchodilator spirometry, the test report must explain why. We can use the results of spirometry administered without bronchodilators when the use of bronchodilators is medically contraindicated.
c. Your forced expiratory maneuvers must be satisfactory. We consider a forced expiratory maneuver to be satisfactory when you exhale with maximum effort following a full inspiration, and when the test tracing has a sharp takeoff and rapid rise to peak flow, has a smooth contour, and either lasts for at least 6 seconds or maintains a plateau for at least 1 second.
3. The spirometry report must include the following information:
a. The date of the test and your name, age or date of birth, gender, and height without shoes. (We will assume that your recorded height on the date of the test is without shoes, unless we have evidence to the contrary.) If your spine is abnormally curved (for example, you have kyphoscoliosis), we will substitute the longest distance between your outstretched fingertips with your arms abducted 90 degrees in place of your height when this measurement is greater than your standing height without shoes.
b. Any factors, if applicable, that can affect the interpretation of the test results (for example, your cooperation or effort in doing the test).
c. Legible tracings of your forced expiratory maneuvers in a volume-time format showing your name and the date of the test for each maneuver.
4. If we purchase spirometry, the medical source we designate to administer the test is solely responsible for deciding whether it is safe for you to do the test and for how to administer it.
F. What is a DLCO test, and what are our requirements for an acceptable test and report?
1. A DLCO test measures the gas exchange across cell membranes in your lungs. It measures how well CO diffuses from the alveoli (air sacs) of your lungs into your blood. DLCO may be severely reduced in some disorders, such as interstitial lung disease (for example, idiopathic pulmonary fibrosis, asbestosis, and sarcoidosis) and COPD (particularly emphysema), even when the results of spirometry are not significantly reduced. We use the average of two of your unadjusted (that is, uncorrected for hemoglobin concentration) DLCO measurements reported in mL CO (STPD)/min/mmHg to evaluate your respiratory disorder under C1.
2. We have the following requirements for DLCO tests under these listings:
a. You must be medically stable at the time of the test. See E2a.
b. The test must use the single-breath technique.
(i) The VI during the DLCO maneuver must be at least 85 percent of your current FVC, and your time of inhalation must be less than 4 seconds. (See E for our rules for programmatically acceptable spirometry.) If you do not have an FVC measurement on the same day as the DLCO test, we may use your FVC from programmatically acceptable spirometry administered within 90 days of the DLCO test.
(ii) Your breath-hold time must be between 8 and 12 seconds.
(iii) Your total exhalation time must be less than or equal to 4 seconds, with a sample collection time of less than 3 seconds. If your FVC is at least L, the washout volume must be between L and L. If your FVC is less than L, the washout volume must be at least L.
3. The DLCO test report must include the following information:
a. The date of the test and your name, age or date of birth, gender, and height without shoes. (We will assume that your recorded height on the date of the test is without shoes, unless we have evidence to the contrary.) If your spine is abnormally curved (for example, you have kyphoscoliosis), we will substitute the longest distance between your outstretched fingertips with your arms abducted 90 degrees in place of your height when this measurement is greater than your standing height without shoes.
b. Any factors, if applicable, that can affect the interpretation of the test results (for example, your cooperation or effort in doing the test).
c. Legible tracings of your VI, breath-hold maneuver, and volume of exhaled gas showing your name and the date of the test for each DLCO maneuver.
d. At least two acceptable (see F2) DLCO measurements within 3 mL CO (STPD)/min/mmHg of each other or within 10 percent of the highest value.
4. We may need to purchase a DLCO test to determine whether your disorder meets C1 when we have evidence showing that you have a chronic respiratory disorder that could result in impaired gas exchange, unless we can make a fully favorable determination or decision on another basis. Since the DLCO calculation requires a current FVC measurement, we may also purchase spirometry at the same time as the DLCO test, even if we already have programmatically acceptable spirometry.
5. Before we purchase a DLCO test, a medical consultant (see §§ and of this chapter), preferably one with experience in the care of people with respiratory disorders, must review your case record to determine if we need the test. The medical source we designate to administer the test is solely responsible for deciding whether it is safe for you to do the test and for how to administer it.
G. What is an ABG test, and what are our requirements for an acceptable test and report?
1. General. An ABG test measures PaO2, PaCO2, and the concentration of hydrogen ions in your arterial blood. We use a resting or an exercise ABG measurement to evaluate your respiratory disorder under C2.
2. Resting ABG tests.
a. We have the following requirements for resting ABG tests under these listings:
(i) You must be medically stable at the time of the test. See E2a.
(ii) The test must be administered while you are breathing room air; that is, without oxygen supplementation.
b. The resting ABG test report must include the following information:
(i) Your name, the date of the test, and either the altitude or both the city and State of the test site.
(ii) The PaO2 and PaCO2 values.
c. We may need to purchase a resting ABG test to determine whether your disorder meets C2 when we have evidence showing that you have a chronic respiratory disorder that could result in impaired gas exchange, unless we can make a fully favorable determination or decision on another basis.
d. Before we purchase a resting ABG test, a medical consultant (see §§ and of this chapter), preferably one with experience in the care of people with respiratory disorders, must review your case record to determine if we need the test. The medical source we designate to administer the test is solely responsible for deciding whether it is safe for you to do the test and for how to administer it.
3. Exercise ABG tests.
a. We will not purchase an exercise ABG test.
b. We have the following requirements for exercise ABG tests under these listings:
(i) You must have done the exercise under steady state conditions while breathing room air. If you were tested on a treadmill, you generally must have exercised for at least 4 minutes at a grade and speed providing oxygen (O2) consumption of approximately milliliters per kilogram per minute (mL/kg/min) or metabolic equivalents (METs). If you were tested on a cycle ergometer, you generally must have exercised for at least 4 minutes at an exercise equivalent of METs.
(ii) We may use a test in which you have not exercised for at least 4 minutes. If you were unable to complete at least 4 minutes of steady state exercise, we need a statement by the person administering the test about whether the results are a valid indication of your respiratory status. For example, this statement may include information about your cooperation or effort in doing the test and whether you were limited in completing the test because of your respiratory disorder or another impairment.
c. The exercise ABG test report must include the following information:
(i) Your name, the date of the test, and either the altitude or both the city and state of the test site.
(ii) The PaO2 and PaCO2 values.
H. What is pulse oximetry, and what are our requirements for an acceptable test and report?
1. Pulse oximetry measures SpO2, the percentage of oxygen saturation of blood hemoglobin. We use a pulse oximetry measurement (either at rest, during a 6MWT, or after a 6MWT) to evaluate your respiratory disorder under C3 or, if you have CF, to evaluate it under F.
2. We have the following requirements for pulse oximetry under C3:
a. You must be medically stable at the time of the test. See E2a.
b. Your pulse oximetry measurement must be recorded while you are breathing room air; that is, without oxygen supplementation.
c. Your pulse oximetry measurement must be stable. By “stable,” we mean that the range of SpO2 values (that is, lowest to highest) during any second interval cannot exceed 2 percentage points. For example: (1) The measurement is stable if the lowest SpO2 value during a second interval is 87 percent and the highest value is 89 percent—a range of 2 percentage points. (2) The measurement is not stable if the lowest value is 86 percent and the highest value is 89 percent—a range of 3 percentage points.
d. If you have had more than one measurement (for example, at rest and after a 6MWT), we will use the measurement with the lowest SpO2 value.
e. The pulse oximetry report must include the following information:
(i) Your name, the date of the test, and either the altitude or both the city and State of the test site.
(ii) A graphical printout showing your SpO2 value and a concurrent, acceptable pulse wave. An acceptable pulse wave is one that shows the characteristic pulse wave; that is, sawtooth-shaped with a rapid systolic upstroke (nearly vertical) followed by a slower diastolic downstroke (angled downward).
f. We may need to purchase pulse oximetry at rest to determine whether your disorder meets C3 when we have evidence showing that you have a chronic respiratory disorder that could result in impaired gas exchange, unless we can make a fully favorable determination or decision on another basis. We may purchase pulse oximetry during and after a 6MWT if your SpO2 value at rest is greater than the value in Table V.
g. Before we purchase pulse oximetry, a medical consultant (see §§ and of this chapter), preferably one with experience in the care of people with respiratory disorders, must review your case record to determine if we need the test. The medical source we designate to administer the test is solely responsible for deciding whether it is safe for you to do the test and for how to administer it.
3. We have the following requirements for pulse oximetry under F:
a. You must be medically stable at the time of the test. See E2a.
b. Your pulse oximetry measurement must be recorded while you are breathing room air; that is, without oxygen supplementation.
c. If you have had more than one measurement (for example, at rest and after a 6MWT), we will use the measurement with the lowest SpO2 value.
d. The pulse oximetry report must include your name, the date of the test, and either the altitude or both the city and State of the test site. If you have CF, we do not require a graphical printout showing your SpO2
Failure Behavior of Hot-Dry-Rock (HDR) in Enhanced Geothermal Systems: Macro to Micro Scale Effects
References
- R. G. S. Araújo, J. L. A. O. Sousa, and M. Bloch, “Experimental investigation on the influence of temperature on the mechanical properties of reservoir rocks,” International Journal of Rock Mechanics & Mining Sciences, vol. 34, no. 3–4, pp. e1–, View at: Publisher Site | Google Scholar
- S. J. Bauer and J. Handin, “Thermal expansion and cracking of three confined water-saturated igneous rocks to °C,” Rock Mechanics & Rock Engineering, vol. 16, no. 3, pp. –, View at: Publisher Site | Google Scholar
- R. D. Dwivedi, R. K. Goel, V. V. R. Prasad, and A. Sinha, “Thermo-mechanical properties of Indian and other granites,” International Journal of Rock Mechanics & Mining Sciences, vol. 45, no. 3, pp. –, View at: Publisher Site | Google Scholar
- Y. Mahmutoglu, “Mechanical behaviour of cyclically heated fine grained rock,” Rock Mechanics & Rock Engineering, vol. 31, no. 3, pp. –, View at: Publisher Site | Google Scholar
- J. Fan, P. Liu, J. Li, and D. Jiang, “A coupled methane/air flow model for coal gas drainage: model development and finite-difference solution,” Process Safety and Environmental Protection, vol. , pp. –, View at: Publisher Site | Google Scholar
- A. Liu, S. Liu, X. Hou, and P. Liu, “Transient gas diffusivity evaluation and modeling for methane and helium in coal,” International Journal of Heat and Mass Transfer, vol. , article , View at: Publisher Site | Google Scholar
- Z. Feng, Y. Zhao, Y. Zhang, and Z. Wan, “Real-time permeability evolution of thermally cracked granite at triaxial stresses,” Applied Thermal Engineering, vol. , pp. –, View at: Publisher Site | Google Scholar
- C. Goetze, “High temperature rhelogy of westerly granite,” Journal of Geophysical Research, vol. 76, no. 5, pp. –, View at: Publisher Site | Google Scholar
- F. E. Heuze, “High-temperature mechanical, physical and Thermal properties of granitic rocks-- A review,” International Journal of Rock Mechanics & Mining Sciences & Geomechanics Abstracts, vol. 20, no. 1, pp. 3–10, View at: Publisher Site | Google Scholar
- S. Kou, “Effect of thermal cracking damage on the deformation and failure of granite,” Acta Mechanica Sinica, vol. , pp. –, View at: Google Scholar
- S. Liu and J. Xu, “An experimental study on the physico-mechanical properties of two post-high- temperature rocks,” Engineering Geology, vol. , no. 4, pp. 63–70, View at: Publisher Site | Google Scholar
- I. van der Molen, “The shift of the α-β transition temperature of quartz associated with the thermal expansion of granite at high pressure,” Tectonophysics, vol. 73, no. 4, pp. –, View at: Publisher Site | Google Scholar
- Q. Sun, W. Zhang, L. Xue, Z. Zhang, and T. Su, “Thermal damage pattern and thresholds of granite,” Environmental Earth Sciences, vol. 74, no. 3, pp. –, View at: Publisher Site | Google Scholar
- Z. Wan, Y. Zhao, F. Dong, Z. Feng, N. Zhang, and J. Wu, “Experimental study on mechanical characteristics of granite under high temperatures and triaxial stresses,” Chinese Journal of Rock Mechanics & Engineering, vol. 27, no. 1, pp. 72–77, View at: Google Scholar
- T. F. Wong, “Effects of temperature and pressure on failure and post-failure behavior of westerly granite,” Mechanics of Materials, vol. 1, no. 1, pp. 3–17, View at: Publisher Site | Google Scholar
- Y. S. Zhao, Z. J. Wan, Z. J. Feng, Z. H. Xu, and W. G. Liang, “Evolution of mechanical properties of granite at high temperature and high pressure,” Geomechanics and Geophysics for Geo-Energy and Geo-Resources, vol. 3, no. 2, pp. –, View at: Publisher Site | Google Scholar
- R. L. Kranz, “Microcracks in rocks: a review,” Tectonophysics, vol. , no. , pp. –, View at: Publisher Site | Google Scholar
- X. Xu, Z. Kang, M. Ji, W. Ge, and J. Chen, “Research of microcosmic mechanism of brittle-plastic transition for granite under high temperature,” Procedia Earth & Planetary Science, vol. 1, no. 1, pp. –, View at: Publisher Site | Google Scholar
- H. Zhu, Z. Yan, T. Deng, J. Yao, L. Zeng, and J. Qiang, “Testing study on mechanical properties of tuff, granite and breccia after high temperatures,” Chinese Journal of Rock Mechanics & Engineering, vol. 25, no. 10, pp. –, View at: Google Scholar
- S. Yin, R. Shu, X. Li, P. Wang, and X. Liu, “Comparison of mechanical properties in high temperature and thermal treatment granite,” Transactions of Nonferrous Metals Society of China, vol. 26, no. 7, pp. –, View at: Publisher Site | Google Scholar
- L. P. Zhi, J. Y. Xu, J. Z. Jin, S. Liu, and T. F. Chen, “Research on ultrasonic characteristics and mechanical properties of granite under post-high temperature,” Chinese Journal of Underground Space and Engineering, vol. 8, no. 4, pp. 54–59, View at: Google Scholar
- Y. Chen, W. Shao, and Y. Zhou, “Experimental study on mechanical properties of granite after high temperature,” Chinese Quarterly of Mechanics, vol. 32, no. 3, pp. –, View at: Google Scholar
- B. Xi and Y. Zhao, “Experimental research on mechanical properties of water-cooled granite under high temperatures within °C,” Chinese Journal of Rock Mechanics & Engineering, vol. 29, no. 5, pp. –, View at: Google Scholar
- S. J. Du, H. Liu, H. T. Zhi, and H. H. Chen, “Testing study on mechanical properties of post-high-tempearture granite,” Chinese Journal of Rock Mechanics & Engineering, vol. 23, no. 14, pp. –, View at: Google Scholar
- Y. L. Chen, S. R. Wang, J. Ni, R. Azzam, and T. M. Fernández-steeger, “An experimental study of the mechanical properties of granite after high temperature exposure based on mineral characteristics,” Engineering Geology, vol. , pp. –, View at: Publisher Site | Google Scholar
- S. Q. Yang, P. G. Ranjith, H. W. Jing, W. L. Tian, and Y. Ju, “An experimental investigation on thermal damage and failure mechanical behavior of granite after exposure to different high temperature treatments,” Geothermics, vol. 65, pp. –, View at: Publisher Site | Google Scholar
- G. M. N. Rao and C. R. Murthy, “Dual role of microcracks: toughening and degradation,” Canadian Geotechnical Journal, vol. 38, no. 2, pp. –, View at: Publisher Site | Google Scholar
- L. Griffiths, O. Lengliné, M. J. Heap, P. Baud, and J. Schmittbuhl, “Thermal cracking in westerly granite monitored using direct wave velocity, coda wave interferometry and acoustic emissions,” Journal of Geophysical Research Solid Earth, vol. , no. 3, pp. –, View at: Publisher Site | Google Scholar
- J. Browning, P. Meredith, and A. Gudmundsson, “Cooling-dominated cracking in thermally stressed volcanic rocks,” Geophysical Research Letters, vol. 43, no. 16, pp. –, View at: Publisher Site | Google Scholar
- K. Kim, J. Kemeny, and M. Nickerson, “Effect of rapid thermal cooling on mechanical rock properties,” Rock Mechanics & Rock Engineering, vol. 47, no. 6, pp. –, View at: Publisher Site | Google Scholar
- C. V. Raman and T. M. K. Nedungadi, “The α-β transformation of quartz,” Nature, vol. , no. , pp. –, View at: Publisher Site | Google Scholar
- Y. Chen, D. Li, Q. Jiang, and C. Zhou, “Micromechanical analysis of anisotropic damage and its influence on effective thermal conductivity in brittle rocks,” International Journal of Rock Mechanics & Mining Sciences, vol. 50, no. 2, pp. –, View at: Publisher Site | Google Scholar
- Y. Zhao, Q. Meng, T. Kang, N. Zhang, and B. Xi, “Micro-ct experimental technology and meso-investigation on thermal fracturing characteristics of granite,” Chinese Journal of Rock Mechanics & Engineering, vol. 27, no. 1, pp. 28–34, View at: Google Scholar
- L. Griffiths, M. J. Heap, P. Baud, and J. Schmittbuhl, “Quantification of microcrack characteristics and implications for stiffness and strength of granite,” International Journal of Rock Mechanics Mining Sciences, vol. , pp. –, View at: Publisher Site | Google Scholar
- G. Dolino and J. P. Bachheimer, “Fundamental and second-harmonic light scattering by the α-β coexistence state of quartz,” Physica Status Solidi, vol. 41, no. 2, pp. –, View at: Publisher Site | Google Scholar
- S. Kume and N. Kato, “A furnace for high-temperature X-ray diffraction topography,” Journal of Applied Crystallography, vol. 7, no. 4, pp. –, View at: Publisher Site | Google Scholar
- C. M. E. Zeyen, G. Dolino, and J. P. Bachheimer, “Neutron and calorimetric observation of a modulated structure in quartz just above the α-β phase transition,” Physica B+C, vol. , no. , pp. –, View at: Publisher Site | Google Scholar
- J. T. Fredrich and T. Wong, “Micromechanics of thermally induced cracking in three crustal rocks,” Journal of Geophysical Research Solid Earth, vol. 91, no. B12, pp. –, View at: Publisher Site | Google Scholar
- Z. Zhang, F. Gao, and X. Xu, “Experimental study of temperature effect of mechanical properties of granite,” Rock and Soil Mechanics, vol. 32, no. 8, pp. –, View at: Google Scholar
- S. Shao, P. G. Ranjith, P. L. P. Wasantha, and B. K. Chen, “Experimental and numerical studies on the mechanical behaviour of Australian Strathbogie granite at high temperatures: an application to geothermal energy,” Geothermics, vol. 54, no. 54, pp. 96–, View at: Publisher Site | Google Scholar
- Y. Zhao, Z. Feng, Y. Zhao, and Z. Wan, “Experimental investigation on thermal cracking, permeability under HTHP and application for geothermal mining of HDR,” Energy, vol. , pp. –, View at: Publisher Site | Google Scholar
- A. Korinets and H. Alehossein, “Technical note on the initial non-linearity of compressive stress-strain curves for intact rock,” Rock Mechanics & Rock Engineering, vol. 35, no. 4, pp. –, View at: Publisher Site | Google Scholar
- S. Zhai, G. Wu, Y. Zhang, C. Luo, and Y. Li, “Research on acoustic emission characteristics of granite under high temperature,” Chinese Journal of Rock Mechanics & Engineering, vol. 32, no. 1, pp. –, View at: Google Scholar
- M. Sarfarazi and S. K. Ghosh, “On the micromechanical theories of stressinduced cleavage microcracking in crystalline solids,” Engineering Fracture Mechanics, vol. 27, no. 2, pp. –,
Pp2. Support APFS data recovery and encrypted APFS data recoveryppiBoysoft Data Recovery for Mac is one of a few APFS data recovery that can recover lost data from encrypted APFS drive, recover lost data from formatted, inaccessible, corrupted, unreadable, unmountable APFS drive. pp3. Powerful preview functionppiBoysoft Data Recovery for Mac can preview documents, photos, videos, audios, etc.
file types that our Mac computers support to preview.
.What’s New in the 20/200 2.2 serial key or number?
Screen Shot
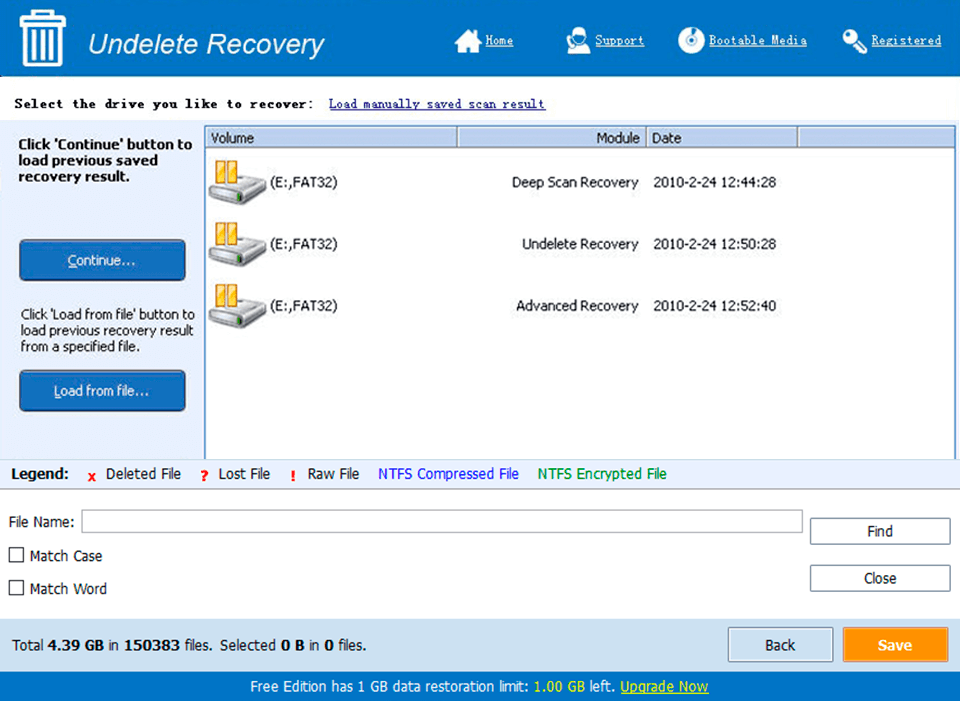
System Requirements for 20/200 2.2 serial key or number
- First, download the 20/200 2.2 serial key or number
-
You can download its setup from given links:


